17/3 By Dr. Sipko van Dam
Preventive health interventions can increase health span
Average life expectancy in the Netherlands has increased to 82 years over the past decades. But the average health span – the number of years during which a person can expect to enjoy good health – is only 61, meaning the majority of elderly people live their later years suffering from chronic conditions. What can policymakers do about it?

The challenges
Traditionally, healthcare professionals and policymakers have viewed the increase in life expectancy as a positive thing, an indication of successful care outcomes.
But since the gap between life expectancy and health span has grown larger, people are mostly extending the part of their lives lived in poor health.
The healthcare system faces a ticking time bomb in the years ahead as it will struggle to cope with ever-increasing demand for diagnosis and treatment, partly driven by the growing prevalence of unhealthy lifestyles, even among the younger generations.
Consider that 48% of the Dutch population do not exercise sufficiently, 20% smoke, 16% suffer from burn-out complaints, and less than 10% follow the public health institute (RIVM) recommended diet. The average individual spends three hours a day watching television, with teenagers spending an additional three hours daily playing computer games and using social media channels.
As a result of these behavior patterns, the increasing need for treatment is having a direct impact on the cost of healthcare in the Netherlands, widening the gap between and the young and the old, and the rich and the poor in our society.
What drives healthcare inflation?
Since 1998, average monthly healthcare costs per person have more than tripled, from approximately €150 per month to more than €500. And these monthly costs are expected to rise to beyond €800 by 2040.
But what is driving the increase? Within the current health care system, care is often used incorrectly or unnecessarily for several reasons.
Nobody is responsible for prevention.
When people have minor health complaints, there are currently two solutions available. They either do nothing until they need urgent medical attention, or they partake in an elaborate treatment. An additional avenue is needed to support those who do not have serious health problems but are not perfectly healthy either. This is where preventive care can offer a solution. employee sick leave.
Unnecessary referrals blocking the system.
As a result of the fact that there are no avenues available for people to take preventive or early action, people with minor care needs are often wrongly referred to specialized care, which means that patients with serious conditions, who need care the most, are put on waiting lists, causing unnecessary blockages in the system.
Time pressures in primary care.
The current system revolves around treating disease, as doctors do not have enough time to motivate people to lead a healthier lifestyle. Medicine requires only a single interaction with the patient and is therefore faster in each individual case, yet more expensive collectively over the long term.
Poorly designed incentives.
Healthcare providers are often incentivized to provide more care or diagnostics than is really necessary. For example, expensive MRI scans may be ordered for people with minor back pain, causing unnecessary anxiety – and also contributing to healthcare inflation.
One of the solutions to rising costs is for policymakers to start to communicate to the public about how individuals can take action to avoid preventable illnesses while they are still in good health.
While the health literacy of the general public is limited, citizens’ general interest in health has been heightened as a result of the global pandemic, as it illustrates the fact that people with chronic illness or pre-existing conditions are more vulnerable to suffer long-term complications, such as chronic fatigue. Therefore, all stakeholders have a rare window of opportunity to capitalize on a highly engaged public.
Prioritizing healthy life years
Rather than making incremental changes to the existing healthcare model, what would happen if policymakers pivoted towards prevention?
In response to the challenges facing healthcare delivery, many organizations such as the World Health Organization, the Dutch government and the Eurostat commission are making ‘healthy life years’ a strategic priority.
Healthy life years can be defined as years lived without longstanding illnesses such as diabetes or heart disease.
At Ancora Health, our ambition is to add 5 million healthy life years to the society by 2030, working with multiple stakeholders to dampen down the rise in health costs and ultimately bring a better quality of life to citizens as they grow older.
Researching the benefits of healthy life years

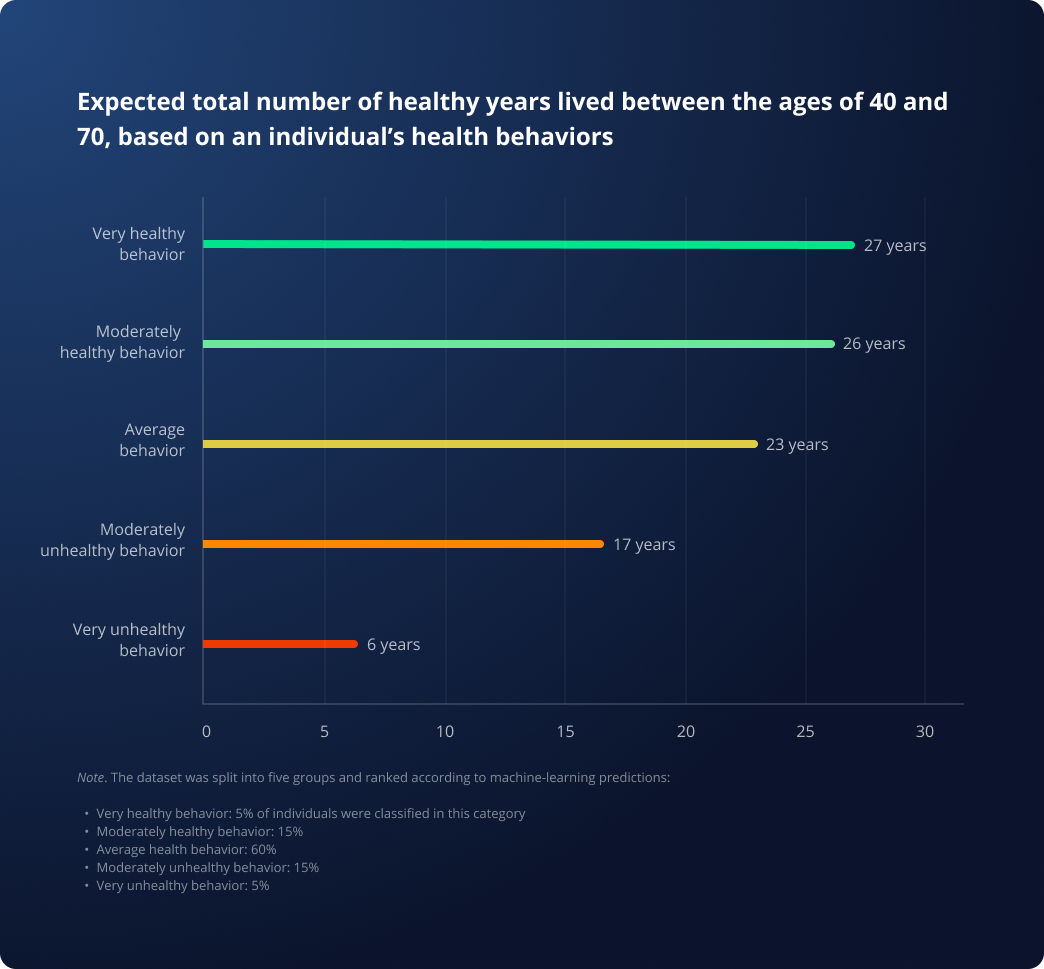
Thanks to the rapid advancement of data collection methods, our research team has been able to quantify the benefits of good behavioral health choices on the number of healthy life years lived.
In collaboration with the University Medical Center Groningen, we used machine learning, a branch of artificial intelligence, to examine the relationships between people’s genetics, diet, behavior and the resulting health outcomes as they grow older.
Methodology
Machine learning is only effective when applied to large sets of data. For this reason, we analyzed large datasets from the UK Biobank and Lifelines. These troves of data contain information from hundreds of thousands of volunteers who gave blood samples, physical measurements and answers to thousands of questions on their health history and lifestyle.
We identified links between people’s health behaviors and health outcomes, the relationship between lifestyle and physical health and how this impacts the probability of a person becoming chronically ill.
Specifically, we considered the following factors to identify links between lifestyle choices and health outcomes:
- Smoking status
- Perceived stress level
- Sleep quality
- Time spent watching TV or playing computer games
- Physical activity
- Walking speed
- Diet
- Alcohol consumption
Key findings from our research
The main conclusion from our research is not surprising. People with unhealthy lifestyles are more likely to live their later years in an unhealthy state, translating into fewer healthy life years.
Highlights from the dataset analysis:
- Individuals that have a poor lifestyle on average live only 4 years in a healthy state between the ages of 40 and 70, rather than the full 30 years one would hope for.
- The healthiest group of individuals – i.e. those who score well in terms of healthy behaviors – live on average 25 healthy life years between the ages of 40 and 70.
- People in the unhealthiest group (5% unhealthiest) have 6 BMI points more than those in the healthiest group (5% healthiest).
Looking to the future
Since doctors are likely to become even more occupied in the future, with more patients and more possible treatments, it is important to transfer the burden of choosing and execution of interventions to other experts, such as health coaches, or even to individuals themselves, where possible.
If people could become aware of possible treatment alternatives, such as remitting type-2 diabetes through lifestyle interventions, they could take control of their health themselves and solve a complaint before it becomes chronic, rather than maintaining a permanent state of disease.
At Ancora, this is the approach we are pioneering. We are developing tools that allow not only doctors, but also individuals, to have access to information about their health risks, in an easily interpretable manner.
We strongly believe that if citizens can better understand the potential benefits of preventive health, such as remitting type-2 diabetes through lifestyle interventions, that could increase their likelihood of enjoying a longer health span.
To help drive the change, government policy can also play its role in empowering people to make better health choices. For example, subsidies for healthy goods such as fruit and vegetables could be offset by the introduction of taxes on unhealthy goods such as sugar.
Experience from our preventive health programs
For the average person that participates in our preventive health programs, having access to their own health data in an easy-to-understand format proves to be empowering.
We observe that when people are made aware of their personal health risks, they have an objective data point to take decisions on how to reduce those risks, as well as to measure their progress over time.
But we also see that to really drive sustainable health outcomes over the long term, people need guidance, coaching and motivational support.
That is why we coach people to tackle their health challenges in areas such as nutrition, exercise, mental health and micro-habits that support behavior change. We also integrate wearable data, such as heart rate tracking and electronic weighing scales into our platform, so people can track the progress they are making.
Since our platform integrates many layers of data, we see the potential to correlate the effects of coaching with health status, and eventually outcomes.
As our platform gives full control to the individual as well as supplying them with meaningful interpretations of their data our approach has the potential to outperform current reactive care methods.
Financial considerations
While the benefits of preventive health interventions are starting to be better understood, the cost to the user remains a key consideration. Our experience shows that only a small percentage of individuals are willing to invest their own money in preventive health.
What are the possible solutions? One could be a scheme whereby either insurance providers or government makes a commitment to invest in preventive health programs.
This is much more likely to happen if the long-term financial gain for the payer is clear.
Modelling the cost savings achievable through the application of preventive health
The high cost of chronic care can be at least partly reduced through preventive care. Ideally, preventive care should be targeted towards those who have the largest risk probability for chronic disease, applying the appropriate preventive measures for the condition the person is at highest risk for. For example, preventive measures for type-2 diabetes are very different from the measure effective against depression.
At Ancora, we have made preliminary efforts to model the financial payoff of preventive interventions. For effective modelling, the use of large datasets is paramount. From the data we have analyzed from the UK Biobank and Lifelines, we observe that it is possible to identify individuals who have a 10-fold higher risk for certain health outcomes based on questionnaire data alone. Since these high-risk individuals are likely to become a heavy burden on the healthcare system, it would be cost effective to apply follow-up screening to this cohort.
While follow-up screening is more costly, it is worthwhile as a large number of these individuals will likely be on track to develop disease, and some may already have it. Early diagnosis would reduce the impact of disease, resulting in a benefit to the patient and also their insurance provider.
Meanwhile, those who are rapidly heading towards disease could be targeted for preventive interventions. Our research suggests that applying this approach could ultimately add 20 extra healthy life years to the unhealthiest population group. Since healthcare costs are far highest for the least healthy, this approach could alleviate the financial pressure on the healthcare system.
In an ideal scenario, one central system where all data from each individual in the Netherlands is recorded would be used to make such calculations. At Ancora, we are exploring the possibilities of such an integrated data system in the Netherlands.
In summary
-
To tackle the root causes of poor health span, policymakers should create the conditions that empower individuals to take control of their own health. Only then will we keep healthcare affordable and make sure people enjoy a high quality of life as they grow older.
-
People have the chance to extend their health span if they improve the lifestyle factors within their personal control, such as diet and physical activity. Even simple changes, such as spending less time sitting on the sofa, could tip the balance towards a person enjoying significantly more healthy life years.
-
Nevertheless, the pursuit of longer health span is not a one-size-fits-all endeavor. It relies upon identifying key risk factors for each individual and translating this into realistic lifestyle improvement actions aligned with the person’s needs, goals and preferences.
As one of Europe’s leading preventive health specialists, Ancora offers a range of health programs for employers. Our mission is to empower people to take ownership of their (mental) health, wellbeing and performance by combining the power of the most advanced science, data and technology into a personalized program that delivers positive health outcomes.
SUBSCRIBE
Subscribe to our mailing list to be among the first to know about our latest blogs.
Learn how Ancora handles your personal data in our privacy policy