8/2/23 By Jeroen Tas and Sven Hermans
The moment for the digital breakthrough in healthcare is now
Long waiting lists. Spiraling costs. Staff shortages. Everyone agrees that the Netherlands is facing a growing healthcare crisis. However, technology has the potential to make care more efficient and effective, and also – as we show at Ancora – play an important role in prevention. A breakthrough in digital healthcare requires initiative from both public and private sectors. It’s time to take bold steps.
We have seen the warning signs for many years. A healthcare crisis is coming, with uncontrolled waiting lists and overloaded staff. But, as NRC recently wrote, we don’t have to look to the future: The crisis is already happening now.
120,000 Dutch people are waiting longer than normal for operations. There is a shortage of 80,000 workers. Emergency departments are forced to close their doors a few times a day because they are full. The ambulance in which you are rushed to hospital can either wait an hour or drive on to another location. Whether you experience these issues as a patient is a matter of luck.
And now that the crisis is here, there is another, more troubling concern: the system’s capacity to cope with even higher demand. Given the ageing population and increasing demand for care, under reasonable assumptions, one in three employees could be working in the healthcare sector in 40 years’ time, according to the WRR.
One in six employees in the Netherlands already works in healthcare and we spend 11.2 percent of GDP on it, as the Dutch health minister, Ernst Kuipers, wrote in a briefing to the parliament earlier this year. To plan for the future, the country will have to organize healthcare in a smarter way, he explained. “It is unrealistic to assume that the share of healthcare can increase further in the Dutch labor market or on public expenditure.”
With that in mind, the Dutch government has recently signed an Integral Care Agreement (IZA in Dutch) with the national General Practitioners Association, to drive solutions needed to keep healthcare accessible, affordable and of good quality now and in the future. Within the IZA, around €2.8bn has been allocated to “impactful transformations” to strengthen primary care, such as more time for the patient and the new higher rates for evening, night and weekend care.
How to make the transformation happen? Digitization can make an important contribution according to Wouter Bos, CEO of health insurance company Menzis, in a recent radio interview.
Using the example of video consultations, Bos explained that “before Covid, everyone said that video consultations were not feasible at all, but during Covid we found out that they were indeed possible. [Digitization] is a way to provide good care, high-quality care, in an affordable way, without the need for extra people. So that’s really something that we’re going to have to bet really big on.” He added that while patients may prefer to see real people in front of them, “sometimes that can also be done via the video screen; patients don’t have to go to the hospital, so smaller outpatient clinics are needed. In this way we can contribute to solving both a financial and a labor market problem.”
Overcoming inefficiencies
In recent decades, major changes have been achieved in virtually every sector with the help of digital platforms.
With a few clicks you can transfer money internationally, view your financial history from the past 12 months. In the metro you can shop on your mobile phone and the order will arrive the next day. But the transformation in healthcare has proven to be more challenging. Even today, it is rarely possible for patients and their different healthcare providers to easily access the same information and to use these insights for better health outcomes.
Why is digitization in healthcare so difficult? In this article we describe the added value of digitization in healthcare, and the steps that should be taken.
Managing change
Digital transformation is not easy in any industry. It requires intensive cooperation between various parties – sometimes competitors – in the development of protocols and standards. In addition, complex questions about the security and integrity of data must be answered.
In healthcare, the complexity is even greater. The nature of the work means that actors are strongly focused on managing risks and complying with strict regulations in the field of privacy, among other things. That makes collaboration with other healthcare providers challenging.
Digitization is also impeded by the way in which healthcare is currently organized and delivered.
Reimbursements from health insurers are mainly based on services provided such as a consultations, diagnostic tests, medication or procedures, and not on outcomes of the care such as fewer hospital visits by the patient or a faster return to society. In most countries, patient outcomes play a subordinate role. The World Economic Forum calculates that of the 2000 healthcare quality metrics in the US, only 7% relate to patient outcomes. In most business sectors, the work of market parties is largely driven by customer satisfaction. But in healthcare, only 2% of metrics revolve around ‘customers’.
Another challenge is that care is often arranged on the basis of a specific disease. Innovations are driven by these specific services – for example, new therapies or better scanners for doctors to make their diagnoses. Rarely does innovation happen to ensure a better or more convenient experience for patients.
Needless to say, there is an upfront cost to investing in digitization – but this applies to every type of investment.
Policymakers and care providers consider it self-evident to allocate hundreds of millions for the construction of a new hospital or the purchase of new equipment, but it appears harder to structurally invest in digital processes and systems that provide benefits for the entire healthcare sector, perhaps due to the fact that working together is difficult and information technology is less familiar than medical technology.
Advantages of digitalization
Digitalization has so much to offer healthcare. A large part of the doctor-patient interaction can be automated, and this offers a big advantage to care providers and patients.
Think of the time doctors can save if they have quick access to current patient data and insights, including information from other healthcare providers or institutions. Think of the diagnoses that do not have to be repeated and the telephone calls that are no longer necessary. Consider, for example, the possibilities of home monitoring to gain better insight into the situation of patients in their daily lives, to help them with targeted advice, or to intervene in time if a (potential) deterioration occurs.
All of this will drive efficiency in healthcare. According to a report by the consultancy firm Gupta Strategists, digitalization can help to potentially solve existing staff shortages in the Netherlands. Technology, properly deployed, could free up the equivalent of 110,000 employees, nearly as many workers as the Netherlands will be short by 2031.
Likewise, there are huge opportunities in using technology and data to drive continuous improvement. In the traditional care model, there are too few feedback loops or insights into the connection between the care delivered and the patient’s eventual health outcomes. With digitalization, a greater range of actionable data is readily available.
Platforms
A characteristic of digital transformation is that platforms are designed based on customer needs. Because they arise from market demand, platforms can be used to examine where and how certain services can be offered as effectively as possible in an integrated experience with the help of multiple providers. Amazon fulfills consumer needs for housing, food, entertainment, technology and now healthcare. Booking.com fulfills the consumer’s need for vacation.
Platforms bring supply and demand together and take responsibility for orchestrating the services (also from third parties). As healthcare has its own dynamics, however, it doesn’t make sense to build a strategy for platforms purely based on examples from other sectors. As KMPG wrote in a recent report, the supply side in healthcare is more complex than most in terms of regulation, data sharing and financing. The information asymmetry between patients and doctor also makes things more complicated. However, on the demand side, the similarities are many: consumers increasingly want and demand a better experience and want healthcare parties to work better together.
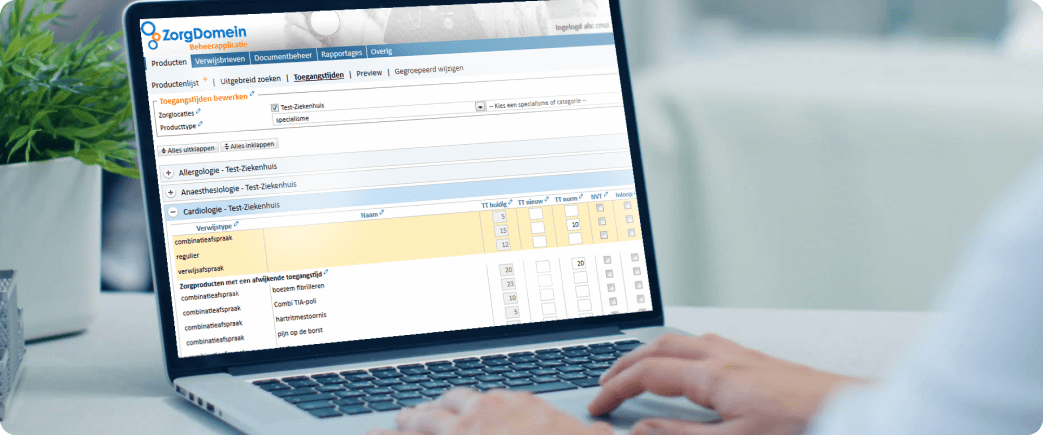
In the world of healthcare, Ancora is an example of a platform focused on the needs of patients. Each patient’s health values are tracked through a mobile app, with data covering weight, diet and amount of exercise. This not only creates a picture of a person’s current fitness, but also creates a baseline for the improvement of health over time. This also applies to those who suffer from chronic diseases and whose behavior influences outcomes. Users can share and discuss the data with medical supervisors such as their GP or lifestyle coach. The aggregated data collected with the app provides valuable information about health trends and the effectiveness of certain interventions and measures.
Prevention
Platforms can play a leading role in preventive health. Sustaining lifestyle improvements is often challenging, but digital solutions help.
Consider the situation of participants in a lifestyle program, such as a digitally supported combined lifestyle intervention (GLI). By seeing their results in an app, they get a better grip on their health. Good behaviors are reinforced. A coach can keep an eye on progress and drive action on the basis of concrete data. The combination of providing insights and active coaching leads to structural progress, based on healthier routines, as shown by several studies carried out by Ancora.
An additional advantage of digitally supported lifestyle programs is that they greatly increase the capacity for these types of interventions, without deploying additional staff. There are some misconceptions about digital lifestyle programs, such as that they are less suitable for many patient groups. But the results show differently. For example, an American study showed that participants in an e-health weight loss program lost the same amount of weight as participants in traditional programs. Participant satisfaction was higher in the e-health group than in the other variant. Online group sessions also yield results comparable to physical groups for people with limited digital literacy, as a systematic review showed.
Moreover, research shows that participants in digitally supported health programs often have a preference for it. A study by C.Journey commissioned by Ancora showed that the target group for a combined lifestyle intervention program has a strong preference for a ‘differentiated’ offer. A digitally supported variant appeals to groups that are otherwise difficult to reach, such as adults aged 30 to 40. With its great flexibility, the digital solution suits people who, for example, have a busy family life or do not have time to travel distances.
For people who live outside the city, have limited mobility, are socially isolated, are socially reluctant or have limited financial means to travel, digital programs are a godsend. And for healthcare providers, supply and demand are better coordinated on a digital platform, because they are not location-bound.

Appropriate care
The Appropriate Care Framework, which the National Health Care Institute presented to the Dutch health minister in June 2022, describes the preconditions that appropriate care must meet. Appropriate care means care that adds sufficient value to people’s lives and has an eye for current social challenges, which is necessary to make care future-proof. “If we do nothing, healthcare threatens to come to a standstill,” the Institute writes.
One of the most important principles is having the right care available in the right place: as close as possible to the patient. And if good digital support is available, that is preferable. “Appropriate care takes place digitally if possible and physically if necessary.” This care must also be tailored to the broader needs of the patient. An elderly man with multiple chronic illnesses, living alone at home, has different needs than a young woman with type I diabetes. This is an important design principle for any platform: the integrated provision of services should fit the needs of the user.
However, in order to support appropriate care digitally, the healthcare sector will have to step up its digital transformation. How to handle that? Institutions and governments can start with concrete initiatives. Doing nothing is not an option given the current problems in healthcare. Hundreds of small projects without a scalable infrastructure and sustainable economic models are also not a solution.
In our view, healthcare institutions should start with regional networks in which they share data with other healthcare providers in order to map out healthcare needs and coordinate their activities. By bringing together information about residents’ health, they can identify inefficiencies in treatment and proactively respond to any problems. This approach can be designed in such a way that value is created for all participants in the ecosystem: better outcomes for patients, more efficient processes, less workload on healthcare, lower total costs for insurers.
Governments can support healthcare by supporting a digital infrastructure where patient data can be shared and analyzed reliably by healthcare providers. The vast majority of Dutch people now indicate that they no longer have any problems sharing their health data. A study by VWS showed that almost all patients surveyed (97%) gave permission for their medical data or bodily material to be used. The role of the government as initiator is important to ensure a coordinated system that meets the highest privacy and data integrity standards.
Scale is important for economic sustainability. Large digital platforms have low marginal costs: additional users can be added at increasingly lower costs. Validated algorithms and programs can be easily distributed. Insights can be quickly aggregated and shared. Covid has taught us that these insights can save lives.
Governments can also play a greater role in stimulating entrepreneurship. New initiatives in healthcare often have to deal with a high burden of proof placed on the effectiveness of medical treatments. However, the example of the DiGA (Digital Health Applications) framework in Germany, and soon also in France, shows that things can be done differently. Entrepreneurs can develop apps and platforms and offer them to patients through a relatively quick approval procedure. Optionally, they may receive temporary approval so that they can decide how to proceed with development based on their initial results. There is no innovation without experimentation.
As in other sectors, digitization can provide healthcare with many efficiencies. And not only efficiency, but also better models. And what it’s all about: better health for citizens.

Jeroen Tas
Jeroen Tas is an entrepreneur and senior executive in healthcare and information technology

Sven Hermans
Sven Hermans is Head of Public Health & Partnerships at Ancora Health