12/12/22 By Jaydev Varma, Head of Product
Transforming care delivery – the role of virtual care
In this blog, we discuss the opportunity for virtual care to transform the current healthcare delivery model, helping to improve population health outcomes and patient experience while reducing costs. Insurance companies, healthcare institutions and health technology organizations should collaborate to make this a reality.
What’s in this blog:
- Chronic problems with the current delivery model
- Introduction to virtual care
- What’s coming next
Dutch healthcare in 2022: a system under stress
If current trends continue, over 50% of the Dutch population may be suffering from chronic illnesses by 2030, up from 32% in 2011. This will place an even greater burden on an already overstretched healthcare system.
While demand for health services outstrips supply, there are currently more than 60,000 job vacancies in the health sector across the Netherlands. Hiring costs are up by 7.7% since 2020. Profitability of hospitals, especially smaller ones, has been dropping year-on- year. Something needs to give.
That said, a lot more can be done with the system’s existing resources, considering that one quarter of healthcare expenditure in the Netherlands is linked to structural inefficiencies such as missed appointments, poor patient management and limited use of digital resources.
Through virtual care, providers can make quality healthcare accessible and affordable for patients across various tiers of care intensity. By enabling appropriate care to be delivered to the right person in the right setting, the system can focus its energies and resources on delivering superior health outcomes at scale and enabling patients to experience a better quality of life.
The role of virtual care
Despite the growth of e-health devices and mobile applications for health and wellness among certain groups, healthcare providers have been slow to recognize the opportunities from leveraging patient-generated data to manage acute or chronic disease in a cost-efficient manner.
Most healthcare services are still delivered in a face-to-face setting, with scheduled visits pegged to the availability of appropriate healthcare professionals, and there is little visibility of user data and self-management during the interim period. It is said that the best predictor of a hospital admission is a previous admission, and part of this can be attributed to the absence of continuity in care.
Consider, for example, a patient diagnosed with heart failure. In the absence of any adverse symptoms or events, the current model involves periodic visits to the cardiologist. A major part of each visit is spent on travel, waiting for the visit, recording historic information if needed, and the rest in providing advice and adjusting medications– ultimately the patient may have limited face time with the cardiologist themselves. But in a virtual care model, the patient can be monitored remotely and can build awareness and self-care skills from the comfort of their own home, supported by digital tools and access to personalized lifestyle coaching; the cardiologist would have a prior/historic view of the issues to discuss or resolve, and the patient would only be brought in for an in-person visit when truly needed.
Similarly, virtual care can help patients prepare for surgical procedures already at home and improve their outcome and experience afterwards. Remote monitoring can also help patients feel reassured that their medical team has early visibility if things are getting worse. And they can empower patients – with insight into their own data – to actively participate in their own recovery plans and thus become part of the solution rather than part of the problem.
Example of virtual care for a patient diagnosed with heart failure
1. After enrollment, patient downloads the virtual care mobile app recommended by the care provider to monitor and improve the diagnosed condition.
2. Patient is dispatched a wearable and other Bluetooth-enabled health devices that connect to the virtual care mobile app.
3. Patient uses the app to track their symptoms. They also read the educational material in the app to improve their awareness and change their lifestyle.
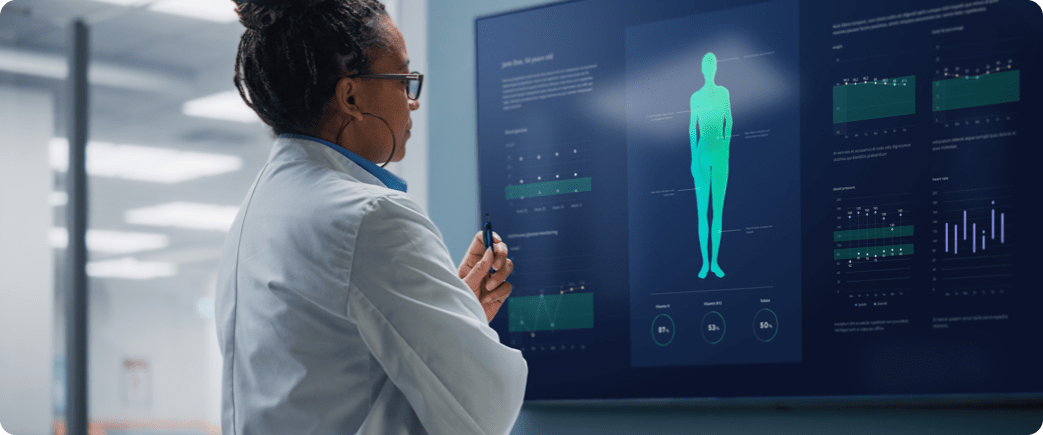
4. The patient’s data and progress are monitored remotely by the care team using the virtual care platform, and the specialists can adjust the care pathway when needed.
5. The care provider can invite the patient for consultations at appropriate moments in order to prevent catastrophic deviations requiring hospitalization.
End result: the right level of care is delivered at the right time and at the right place. The lower care burden is cost effective and convenient for both the patient and the hospital.
Getting off the ground – a work in progress
Despite a slow start, there are exciting virtual care initiatives happening in the Netherlands, which are showing promising results. But there’s a lot more to be done and what we are seeing so far only represents a small part of the actual potential. We will discuss this in more detail in a future post.
But to make virtual care scalable, greater collaboration is urgently needed between all the stakeholders: government, academia, insurers, healthcare providers and health tech companies themselves.
A common and measurable outcome should be a reduction in avoidable healthcare visits, allowing care providers to redeploy scarce resources towards the most pressing challenges.
“Healthcare professionals will always play a vital role in care delivery, and we cannot strip out the ‘human’ element from the equation” says Douwe Atsma, cardiology professor at Leiden University Medical Center. “But imagine how much more effective the whole system will be when healthcare professionals are equipped with intuitive monitoring systems helping them save time, improve patient engagement and achieve better health outcomes. When we think about how the travel industry operated before the advent of online booking tools, this is where we are at right now in healthcare. We are only at the beginning of the curve. The potential for change is infinite.”
That, it must be said, promises to be good news for doctors, patients and healthcare system as a whole.